28 Jan Improving Commercial, Medicaid and Medicare Accountable Care Organizations
The Health Care Transformation Task Force (Task Force) is dedicated to accelerating the transformation of the U.S. health care system to value-based business and clinical models aligned with improving outcomes and lowering costs. To that end, the Task Force developed principles that are important components of successful accountable care payment arrangements and delivery models, and necessary to expanding ACOs beyond their current footprint (Figure 1). These principles fall into three main categories:
1) Honoring Patient Choice, 2) Improving Quality Measurement and 3) Ensuring Financial Stability.
I. Honoring Patient Choice and Improving Attribution
Principle 1: Efforts to meet the Triple Aim are enhanced when an ACO works with an identifiable patient population. Attribution models should support a patient’s ability to actively attest to their participation in a particular ACO.
Beneficiaries should be supported through outreach and education efforts to actively attest to their participation in a particular ACO. Beneficiaries would receive tentative assignment based on historical claims data and would then have the opportunity to confirm attribution through a variety of methods, including through official communications with the payer and in response to direct ACO outreach. After all opportunities for active beneficiary attestation have been exhausted, a passive alignment should take place, utilizing a step-wise, plurality of primary care services methodology where an ACO designates which providers are eligible for “attribution.” In the event that this methodology results in attribution to multiple ACOs, the most recent services should act as the tie-breaker.
II. Quality Measurement Improvement
Principle 1: As ACOs pursue the Triple Aim, payers should create an environment where quality outcomes measurement can be used for more appropriate payment, consumer engagement, and public accountability.
Measurement for Payment
Quality measurement policies and design should create an explicit business case for practicing continuous quality improvement rather than being treated as an initiative, extraneous to the everyday operations of the organization. Essential to creating such an environment is ensuring that all measures that directly affect provider payments be exclusively based on outcomes and be uniform across all payers, both public and private, and all populations such that quality efforts can truly become an integral part of the provider’s work flow. Electronically reporting quality measures to all major payers is also an important part of establishing this industry standard. Additionally, good quality measures will be applicable across the entire population being served and will avoid perpetuating health disparities among varying socioeconomic groups. Providers also recognize that quality measures belong to four distinct categories: 1) clinical, 2) claims-based, 3) patient-experience, and 4) patient-reported. Considering scores and performances as they pertain to a specific category will ensure that care evaluations take into account the many different aspects of what it means to improve health. As these various elements are placed into practice, evidence for which measurements yield the most impact will emerge and those metrics should be emphasized to the exclusion of others. During the early stages of ACO development, it is essential that ACOs demonstrate the ability to improve the quality of care and experience. Metrics in all three domains will be helpful to demonstrate the effectiveness of ACOs. However, using large numbers of more granular metrics for payment can result in distortions in care practices, as well as unforeseen consequences in terms of limiting the sustainability of a model. Therefore, metrics used for payment should be reliably understood, easy to collect without opportunity for gaming, few in number, and indicative of important improvements in health and patient experience of care.
Measurement for Consumer Engagement
To bring to bear market forces on health care, patients must be empowered by quality measures that allow them to identify better performing care providers. In addition to process measures, the use of claims-based and patient-reported measures will facilitate a more comprehensive and accurate evaluation of providers. Under a system that incorporates these additional dimensions, efforts to improve patient-experience surveys and increase participation will become essential. Unlike those used for payment, quality measures for consumer engagement should be designed and scored in a way that allows consumers to compare and evaluate on multiple levels including at the organization, practice and individual provider level. As these measures are further defined and limited to those with the most impact, public reporting requirements will further facilitate their use. Convening a cross-industry group to quickly develop a smaller set of quality metrics emphasizing patient-reported outcomes for use by a number of payers will serve to expedite development, dissemination and adoption.
Measurement for Public Accountability
Measures that are exclusively outcomes-based will provide a way to evaluate whether or not an ACO is actually improving the health of an assigned population and protect against unintended consequences. Measures will need to include both claims and patient-satisfaction data in order to tell the complete story behind care patterns and utilization. ACOs will need real-time access to these monitoring metrics to be able to address organizational shortcomings. Public reporting as a policy will ensure the incentives for addressing organizational deficiencies are always present.
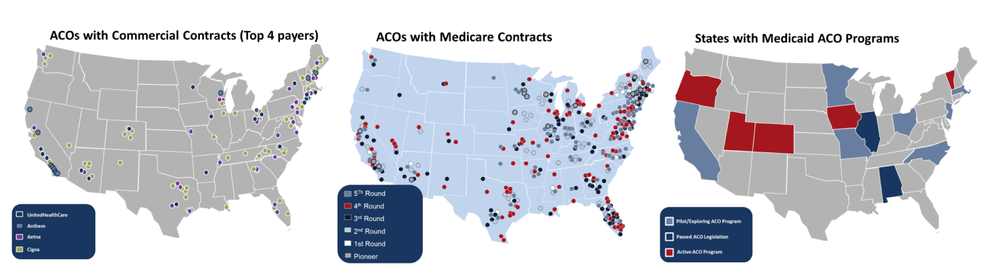
 A breakdown in program size shows that participation in the various private and public sector programs is varied.
A breakdown in program size shows that participation in the various private and public sector programs is varied.
Principle 2: Establish an aligned approach to quality measurement across all three domains of Measurement for Payment, Measurement for Consumer Engagement, and Measurement for Public Accountability.
Using, where possible, nationally endorsed measures will lead to uniformity that providers need. Consistent reporting structures that are maintained at least three years at a time will allow the stability and time necessary for true evaluations. New reporting systems and quality measures without adequate or valid sample sets should fall under a payment-for-reporting structure for the first two years. Additionally, quality measurement programs should allow a minimum of eight weeks for reporting on quality measures.
Principle 3: Explore two statistically-sound quality measurement approaches, establishing a system that rewards both improvement and achievement.
Quality measurement benchmarking methodologies should include aspects that incentivize improvement over prior performance (historical performance) in addition to achievement relative to industry standards (absolute performance). Extra emphasis should be given to reward groups that are able to disproportionately improve conditions and provide high quality care for traditionally disadvantaged populations.
Principle 4: Incentivize ACOs to contribute to emerging/innovative measures.
National quality standards should include efforts to diffuse best practices for quality improvement, such as is done under the auspices of the CMS ACO Learning Network. Incentives should be structured in a way that encourages ACOs to contribute to and refine existing quality measures.
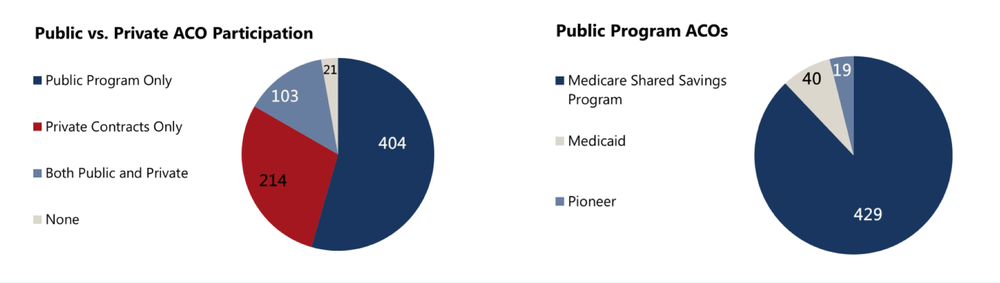
 Growth trend in the adoption of ACOs, overall and broken out on a public versus private basis, has been steady
Growth trend in the adoption of ACOs, overall and broken out on a public versus private basis, has been steady
III. Improving Financial Stability
Principle 1: Simplify the Financial Model.
Payers should offer two statistically sound financial models, designed so that all providers can participate. One should be based on historical claims thereby incentivizing the participation of high-cost providers. The second should be based on community-ratings with health-status adjustments. In developing the latter, local costs/trends should be considered, prospective targets should be set; industry standard risk adjustment models such as the Hierarchical Conditions Categories (HCC) should be utilized and continuously improved. Rebasing methodologies that continuously remove improvements should be eliminated. Financial models should use simple, open-source methods and codes that allow for replicability. Additionally, financial models should, as a rule, carve more care “in” to encourage more comprehensive accountability. For ACOs that do save but are unable to meet the minimum savings rate (MSR), calculations from across the program years should be pooled to recalculate an adjusted MSR.
Principle 2: As ACOs accept more financial risk and demonstrate high-quality care, allow ACOs to better facilitate prospectively-attributed beneficiary receipt of care in appropriate settings.
There is a need to support stronger beneficiary engagement and education regarding covered services and treatment options, including notification and appeals processes for ACOs. Payment policies that determine the site of care for beneficiaries rather than physician judgment should be waived. Additional tools such as information/decision-support tools or tools to encourage care in high value sites should be provided. Fundamental changes to the underlying payment systems to complement the move to full risk, including changes in bundled payments, prepayment, and capitation, should be pursued. We support exploration of financial incentives that support beneficiaries in the management of their health and remove financial barriers to more effective care. Finally, a mechanism should be developed for obtaining feedback regarding allowable practices from an HHS Office of the Inspector General (and other relevant entities).
Principle 3: Continuously improve access to complete, accurate, reliable, timely data.
There is a need to improve reliability and comparability of existing data sets. For delivery systems, a robust process for changing or updating data sets such as test files should be developed. Legislative and/or regulatory changes to remove suppression of mental health and substance-abuse-related claims should be supported. The cost and burden for providers to access, aggregate, and exchange clinical information from their certified electronic health records for population health and care coordination purposes should be reduced. Finally, increased capacity to work across payers to promote comparability of data sets should be supported.
Principle 4: Support transition to triple-aim programs.
The impact of requirements that lead to significant startup costs and administrative burden for those making the transition should be lessened, especially for smaller provider systems and physician groups. ACOs should be financially encouraged to move more quickly to two-sided risk, by providing a higher percent of savings to two-sided risk ACOs and removing the minimum savings and loss rate requirement for two-sided risk ACOs. ACOs should be allowed to retain an MSR to mitigate business risk if they so choose.
