
25 Jun Maternal Health Hub Resources
The Maternal Health Hub compiles resources and best practices to advance a vision for high-value and equitable maternity care in the U.S. The Hub is also home to a learning community for stakeholders committed to improving maternal health outcomes. The Hub is operated by the Health Care Transformation Task Force with support from The Commonwealth Fund.
Promoting Equity and Value in Maternity Care
The Task Force, with support from The Commonwealth Fund, convened a cross-sector group of maternity health experts to identify strategies to accelerate the dissemination of effective value-based payment strategies and delivery models for maternity care. The findings are synthesized in this report: Promoting Equity and Value in Maternity Care. The report outlines a theory of change to chart the path towards a higher-value, more equitable maternity care system. An accompanying blog, Attaining Equitable High-Value Maternity Care, shares the definition and characteristics of high-value maternity care, with equity as a strong foundation, that was developed by the maternity care expert panelists.
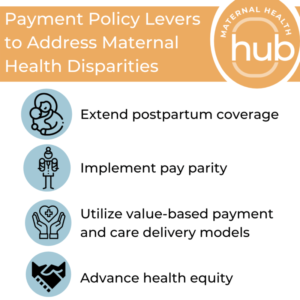
Payment Policy Levers to Address Maternal Health Disparities
 Maternal health outcomes in the U.S. have long signaled systemic inequities for pregnant and birthing persons of color, with Black and Indigenous people two to three times more likely to die in childbirth than white people. Policymakers can take key actions to enact evidence-based payment policies to address maternal health as a top priority.
Maternal health outcomes in the U.S. have long signaled systemic inequities for pregnant and birthing persons of color, with Black and Indigenous people two to three times more likely to die in childbirth than white people. Policymakers can take key actions to enact evidence-based payment policies to address maternal health as a top priority.
The Maternal Health Hub released this report to encourage policymakers to address maternal health disparities by extending postpartum coverage, advocating for pay parity, expanding value-based payment and care delivery, and advancing health equity.
Business Case for Community-Based Maternity Care Models
Community-based maternity care models and support services offer enhanced care from the prenatal through postpartum periods and care coordination that is grounded in reproductive justice. Advancing community-based maternity care and support services can expand access to high-quality, equitable maternity care. This resource is intended to support maternal health stakeholders (e.g., health care providers, birth workers, patient advocates, insurers, and policymakers) in creating a business case to invest in community-based maternity care models and support services from a full complement of birth workers to improve maternal health outcomes and eliminate racial inequities.
The resource serves as a template to assess the current state of maternity care and support services, create a business plan for offering or supporting the development of new maternal health services, and facilitate strategic conversations and planning to establish and support new models, financially or otherwise.
Maternity Care Delivery and Payment Changes During COVID-19: Assessing Equity and Sustaining Innovation
Birthing people, health systems and practitioners had to alter their approach to furnishing care in significant ways in response to COVID-19. These care delivery changes evolved throughout the course of the pandemic alongside knowledge about the transmission and impacts of the virus.
This resource highlights three case studies exploring blended virtual and in-person prenatal care visits, virtual doula and support services, and patient self-advocacy to improve maternal health outcomes. In planning for the post-pandemic maternity care system, it is critical to evaluate the impact of all care delivery models with a health equity lens to determine whether birthing persons of color are benefited or harmed by innovations made in response to the pandemic.
Using Alternative Payment to Transform Maternity Care, Address Disparities in Care, and Improve Outcomes
The Hub Learning Community highlighted efforts to transform maternity care via payment by commercial payers Anthem, Blue Cross Blue Shield of North Carolina (BCBSNC), and the Purchaser Business Group on Health (PBGH); and for the Medicaid populations in Colorado (through Health First Colorado), Tennessee (through TennCare), and the Washington State Health Care Authority (HCA). This resource reflects the learnings shared by these organizations – as well as activities occurring across the country in the public and private sectors as covered in recent literature – on designing and implementing patient-centered, health-equity focused alternative payment models (APMs) with a focus on the following topics:
- Increasing Health Equity and Addressing Social Determinants of Health
- APM Operational Considerations
- APM-Enabling Data and Infrastructure
- Use of Performance Measures for Accountability
